Evaluation Of Effectiveness Of Free Gingival Graft (FGG) For The Escalation Of Gingival
Height By Gingival Thickness Augmentation: A Case Series
Bushra K Quazi 1, M.L.Bhongade 2
A B S T R A C T
INTRODUCTION: Autogenous gingival grafting is a well established pure mucogingival procedure forincreasing the width of keratinized gingiva. This procedure has proven reliable in increasing keratinized gingiva and stopping progressive gingival recession. The long term stability (upto 4 years) of these treatment outcomes has been demonstrated.
METHOD AND MATERIAL: In this case series, 3 cases associated with inadequate width of kerationized gingiva in relation with multiple mandibular anterior teeth were treated by autogenous free gingival graft obtained from palatal region for increasing the width of attached gingiva. For clinical evaluation, all the cases were followed 3 months post-surgically.
RESULTS: 3 months post surgical re evaluation showed an average of mm increase in width of keratinized gingiva. Healing at the donar site was uneventful in all treated cases.
CONCLUSION: The results of the present case series for increasing the width of keratinized gingival and gingival thickness augmentation using free gingival autograft indicate that this procedure could be applied for increasing the width of keratinized gingiva on larger area (2-3 teeth). The free soft gingival autograft when used for increasing the amount of keratinized gingival by escalation of gingival height is a relatively simple surgical procedure.
Introduction :
For many years, the presence of an‘‘adequate’’ amount of gingiva was considered a keystone for the maintenance of periodontal health.1-4 In an observational study, Lang and Loe5 reported that despite the fact that the tooth surfaces were free from plaque, ‘‘all surfaces with less than 2.0 mm of keratinized gingiva exhibited clinical inflammation and varying amounts of gingival exudates.’’ However, a number of authors suggest that sufficient amount of keratinized tissue is considered essential to preserve the healthy periodontal status and to support the
dentogingival unit more resistant during the masticatory function and oral hygiene procedure (Lang and Loe 1972). Therefore the presence of gingival recession associated with a minimal amount or lack of keratinized gingiva may indicate need of gingival augmentation procedure to prevent additional apical displacement of the gingival margin (Agudio 2008,Bertoldi 2007, Camargo et al 2001). In particular, Serino et al.6 showed that sites with gingival recession should be considered susceptible to additional apical displacement of the soft tissue margin. Based on
existing evidence, the American Academy of Periodontology suggested several indications for gingival augmentation procedures: to prevent soft tissue damage in the presence of alveolar bone dehiscence during natural or orthodontic tooth eruption; to halt progressive marginal gingival recession; to improve plaque control and patient comfort around teeth and implants; and to increase the insufficient dimension of gingiva in conjunction withfixed or removable prosthetic dentistry.7
To achieve respectable periodontal esthetics is always an important, yet difficult,but predictable part of practice in periodontology, for which gingival biotype has been the subject of considerable interest amongst periodontists, especially in the last decade. Direct correlation has been suggested to exist between gingival biotype and the susceptibility to gingival recession following surgical and restorative procedures.8 Soft-tissue biotype (gingival thickness) is a critical factor that determines the result of dental treatment. Periodontal surgical procedures can
improve soft-tissue quality resulting in a favorable treatment outcome. Numerous surgical procedures have been advocated to achieve predictable gingival augmentation. Amongst them, autogenous gingival grafting or epithelialized free gingival grafting is a well-established pure mucogingival procedure for increasing the zone of the attached gingival and stopping progressive gingival recession.9
A free gingival graft procedure is one of the most common approaches for gingival augmentation.10-14 This technique accomplishes the following objectives: enhances plaque removal around the gingival margin, reduces gingival inflammation and improves esthetics(Sangnes and gjermo 1976). Some studies reported short- or medium-term data dealing with the stability of the gingival margin after free gingival graft procedures. Very limited data on the position of the gingival margin after the use of free gingival graft over a long period of time is available. Therefore the aim of the present study was to evaluate the effectiveness of free gingival graft for the escalation of gingival height by gingival thickness augmentation.
Method and materials:
A total of 3 patients with age, ranging from 17 –25 years were selected randomly for examination from the outpatient Department of Periodontics, sharad
Pawar dental College Sawangi(Meghe) Wardha. The patients were selected using the following criteria:
Inclusion criteria:
1) Full mouth plaque and bleeding score<20%
2) Presence of atleast one site with complete absence of attached gingival associated with gingival recession and normal sulcus depth
Exclusion criteria:
1) Systemically unhealthy patiens.
2) History of periodontal surgery in selected area.
Prior to initiating of this study, the purpose and diagnostic procedure of this clinical trial was explained to the patients and provided verbal informed consent to participate in the study. The study protocol was first approved by the research and ethical committee of Datta Meghe Institute Of medical Sciences, Sawangi (Meghe), Wardha.
Information concerning dietary status, mouth cleaning habits, systemic background, gingival and periodontal status along with other routine clinical details was recorded . Patients were examined under good illumination with the help of mouth mirror and William’s graduated periodontal probe.
Patient’s oral hygiene was evaluated by using Plaque Index (Turkesy-Gilmore-Glickman Modification of Quigley-Hein, 1970) as an expression of the level of localized mouth supragingival plaque accumulation. Gingival inflammation was assessed by papillary bleeding index (Muhlemann H.R; 1977).
Clinical measurements:
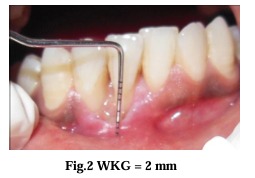
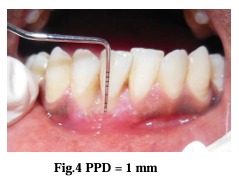
The following measurements were recorded at baseline and 3 months after surgery. – Gingival recession depth (the distance between the gingival margin and the cemento-enamel junction at
the mid-buccal point); – Width of the keratinized gingiva (the distance fromthe gingival margin to the mucogingival junction at themid-buccal point);
– Probing depth at the experimental site (the distance from the gingival margin to the bottom of the gingival sulcus).
Surgical procedure
Preparing the recipient site:
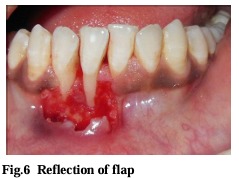
After achieving adequate local anesthesia (2% lignocaine with 1:80,000 adrenaline), the exposed root surface was planed thoroughly with a Gracey 1-2 curette.After obtaining anesthesia, a releasing incision was placed between the mucogingival junction and marginal tissue with a #15 blade. At the level of cemento-enamel junction (CEJ), horizontal incisions were made extending through the line angle of neighbouring teeth on either side of the recession deep into the papilla producing a well defined butt-joint margin. Vertical incisions were given at the terminal ends of the horizontal incision, extending into the alveolar mucosa, so that it is 3 mm beyond the apical extent of the recession. Thus, recipient bed was established, by a partial thickness flap that was reflected (Fig 6) as close to periosteum as possible to create a bed preparation.
Harvesting the free gingival graft from palate:
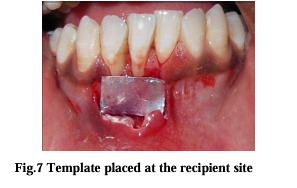
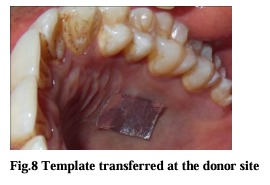
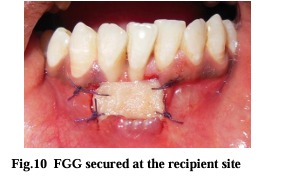
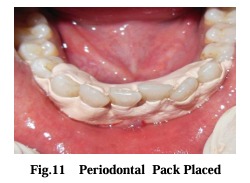
The free gingival graft was harvested from the palate. The goal was to obtain a unform thickness graft approximately 0.75 to 1 mm thick. The amount of donor tissues needed was accurately determined by using a foil template. The template was made by adapting it to the recipient site (Fig 7). The left side of the palate was selected by measuring the thickness of the tissue using an endodontic file with a stopper. The area between the first premolar and first molar (Fig 8) was selected to obtain the desired tissue.The initial incision was outlined by the placement of the tinfoil template with a #15 scalpel blade. All palatal incisions were placed in such a fashion as to make a butt joint. This butt-joint margin of the graft will be butted alongside the butt joint margin in the papilla and the accentuated enamel margins at the cemento-enamel junction. A bevel access incision was made to get an even thickness of the graft. An incision was made along the occlusal aspect of the palate with # 15 scalpel blade held parallel to the tissue, continued apically, lifting and separating the graft. Tissue pliers were used to retract the graft distally as it is being separated apically and dissected, until the graft is totally freed. The graft obtained was inspected for any glandular or fatty tissue remnants. The thickness of the graft was also checked to ensure a smooth and uniform thickness. The harvested graft was placed on the recipient bed, and suture by means of interrupted sutures (4-0 black silk sutures) at the coronal and apical borders (Fig. 9 and 10). A vertical stretching suture was given for close adaption of the graft to the
tooth surface. After suturing a periodontal dressing was placed to protect the surgical site (Fig. 11). The palatal wound was also protected by periodontal dressing and stabilized by Hawley’s retainer already prepared during the pre-surgical phase.
Post- operative care:
Immediately after surgery periodontal dressing was placed on the recipient site and the donor site. After surgery, a non-steroidal anti-inflammatory (Ibugesic-Ibuprofen + Paracetamol B.D for 5 days) was prescribed. No systemic antibiotics were utilized. Patients were instructed not to brush the teeth in the treated area. All patients were placed on 0.2% chlorhexidine gluconate twice daily, for one minute, for 4-6 weeks. They were instructed not to disturb the pack and to avoid to disturb the pack and to avoid undue trauma to the treated site. One week following surgery, periodontal pack was removed. At this time the healing was observed and a second periodontal pack was placed if necessary. After irrigation with saline, polishing was done with the help
of polishing paste and rubber cusp, taking care that it did not traumatize the treated site. Patient were instructed to clean the treated site with cotton pellet saturated with 0.2% chlorhexidine gluconate for additional 3-4 weeks in an apico-coronal direction and later on using a soft tooth brush with Charter’s method of brushing. The patients were recalled at 3 weeks,1 month and 3 months following surgical treatment. At each recall visit, scaling and polishing was performed.
Surgical Photographs:





Results:
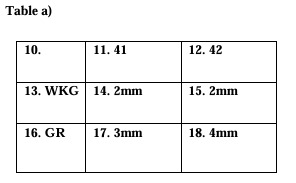
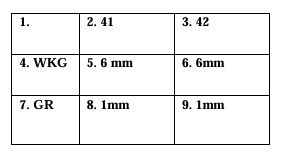
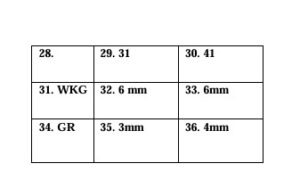
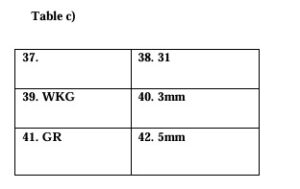
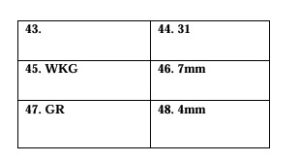
A total of 3 subjects (aged 17 to 25 years) provided sites for gingival augmentation procedures. All sited in this study were treated with free gingival graft positioned apical to the area of recession. There seemed to be significant changes in gingival thickness and height post-operatively after three months as compared to baseline (Tables.a ,b, c). The postoperative increase in width of keratinized gingiva and subsequent gingival augmentation can be appreciated in the figures below. At three months after surgery the amount of keratinized gingiva was increased with mean value 3.07±0.7 mm which was 0.07±0.2 mm at baseline. The mean values of PD remained stable without significant changes.







Discussion:
The aim of the present study was to evaluate the changes in the amount of keratinized gingival and in the position of gingival margin in sites with lack or inadequate zone of attached gingiva after mucogingival treatment by free gingival autografts procedure. Gingival augmentation procedures were performed by placing free gingival grafts at the marginal or submarginal gingival level. The free gingival graft added many dimensions for the correction of mucogingival problems and gingival recession.15,16 The method has been proven to be reliable in increasing attached gingiva and stopping the progressive recession. Root coverage was not the immediate and primary goal of this study. The results showed mean gain of attached gingiva 3.07±0.7 mm. Our clinical observations in this study supported the occurrence of creeping attachment because of the fact that periodontal depth remained stable in all treated sites in the time of the reduction of the recessions. It may be suggested that in cases of shallow recessions this phenomenon can lead to complete root coverage (Rec<3mm, Miller’s class I). The results of this short-term study are
comparable to those reported by Agudio et al., who treated a group of one hundred and three subjects with 224 sites by marginal and submarginal free gingival graft (Agudio et al 2008). In regards to the amount of KT they noted in a retrospective long-term evaluation slight reduction of attached gingival tissue between 1 year and the end of the follow up period (10 to 25 years), whereas the gingival margin shifted coronally. These results they explained with the potential tendency of the mucogingival junction to regain its original position after gingival augmentation
procedure.
The results of the present paper were based on cases with limited follow-up time, and were without controls. Nevertheless, it provides a thought to ponder upon that every millimeter of the biologic tissue is important and every effort should be exercised to augment gingival/soft tissue that may result in prolonging the longevity of the teeth. All the three cases described gingival augmentation in the apical area of tooth and an increase in gingival thickness may, in certain situation, be considered as an endpoint of success. However, further long term randomized clinical trials are required to confirm the hypothesis of gingival height augmentation by augmenting gingival thickness. Further investigations may reveal the influence of different circumstances on the amount of the keratinized gingival tissue gain and recession reduction after free gingival graft treatment.
Conclusion:
In the limits of this study it can be concluded:
1. Free gingival graft augmentation procedure apical to the area of recession is effective in halting the progression of recession in cases associated with an insufficient amount of keratinized tissue and lead to reduction of the whole gingival recession.
2. In cases of shallow recessions (Miller’s class I) this procedure can lead to complete root coverage becauseof the “creeping attachment”.
3. This procedure increases significantly the keratinized tissue and improves esthetics and enhances plaque removal.
4. The free soft gingival autograft when used for increasing the amount of keratinized gingival by escalation of gingival height is a relatively simple surgical procedure.